The Matching Guide has been converted into a published edition of “The Eye Guide.” Please click this link to view the updated information. The contents of this page is now outdated.
The Eye Guide: Matching in Ophthalmology
FREE Digital PDF
Physical Copy from Amazon ($15):
Click the image below to be directed to Amazon (COMING SOON).
Matching in Ophthalmology
Here is the EyeFlyMD Guide to matching in ophthalmology. Opinions are my own and those I’ve solicited from successful applicants over the years. Every individual and experience is different and there are no guarantees in life or in matching so following this guide does not assure a successful outcome. Many I have shared this advice with have found this helpful but you shouldn’t believe everything you read on the internet. Don’t take our word for it.
Contents
Click a section below to jump to it.
Overview of Ophthalmology
Early Considerations
Goals by Year of Medical School
(Away) Rotations
Applications
Interviews and Interview Season
Ranking and Matching
Re-Applying
Additional Resources
Overview of Ophthalmology
Ophthalmology is the best specialty. It’s also unique. It doesn’t use The Electronic Residency Application Service® (ERAS®). It has ascended beyond this and uses SF Match. This means it has an independent timeline from the rest of the specialties and your medical school administration may not be very familiar with it. Everything happens earlier with SF match. Applications are usually submitted by September, Interviews begin shortly thereafter, and match day is early February (vs. March for everyone else).
It’s also undergoing productive changes. Think of all the “lifestyle” specialties that have a preliminary medicine year (dermatology, radiology, anesthesia, etc.). Ophthalmology is doing away with this at many programs and the intern year is integrated, focused on ophthalmology-relevant specialties (ER, rheumatology, dermatology), and not 9 months of ward-based preliminary medicine. Some programs will keep that model but many will be more focused on eyes.
Ophthalmology does benefit an earlier decision and knowing you want to go into it early but it’s completely reasonable to pursue ophthalmology any point during M3 year. It is a fairly competitive specialty (becoming more competitive) but it is also very individualized so special cases occur all the time and weakness in one area should in no way deter you from pursuing the specialty.
Why Ophthalmology is the best
- It’s rapidly changing and extremely innovative, there’s new lenses coming out every few years, there’s the MIGS revolution of the past 10 years, there’s always new promising ways of treating eye disease and it’s always changing, nothing is stagnant.
- There is love and respect for tradition. You learn to use some really cool technology but also your observations during the slit lamp and DFE are absolutely crucial to care. In general medicine accuracy of the physical exam is questionable but in ophthalmology, you are actually visualiIng the optic nerve and retina and making decisions based on your findings.
- It’s people’s vision. Your professional life and free time are largely influenced by your ability to see. This is a really focused field that also makes a HUGE impact on quality of life. Think about how thankful patients are after a routine cataract surgery when everything is suddenly brighter, more vibrant, and clearer.
- The lifestyle is very manageable. It’s a “ROAD” specialty. You can do whatever you want with it. If you want to be part of an academic retina practice and work crazy hours and write textbooks it’s there for you. If you want to do comprehensive ophthalmology and have the same hours as a desk job you can go for it. You don’t really have to take call after residency.
- THERE’S NO ROUNDING, especially in private practice. In residency you’ll have to round on the handful of patients (depending on size of the hospital) who are admitted with eye concerns but you will never be drudging room to room for 5 hours a day and having in depth discussions about sodium status.
- The surgeries are mostly short. Cataracts are 30 minutes in residency and 12 minutes in private practice. Retina, glaucoma, and plastics can go longer and trauma can take hours but your bread and butter is fast. Compare this to a 1 hour appendectomy.
- It’s a small field and everyone knows each other and everyone is incredibly nice. Seriously, ophthalmologists are on average the nicest people I’ve ever worked with. There’s some bad eggs for sure but they’re by far the nicest surgeons I’ve ever met.
- It’s a short residency while still being very specialized. It’s only 4 years.
- Fellowships are still optional. Currently, the only ACGME approved ophthalmology fellowship believe it or not is plastics. You can really shape your own practice. In a bigger city you probably need some fellowship training but everyone still needs a comprehensive ophthalmologist.
Ophthalmology is right for you if
- You love surgery but not general surgery or the “stereotypical” surgery culture.
- You might not have loved what you learned the first two years and are looking for something kind of different than internal medicine.
- You like the idea of heavily specializing while still being able to make huge changes in patients’ lives.
Why you might think twice about Ophthalmology
- It’s fairly competitive with a traditionally high Step 1 score so there’s some gunners out there.
- You are largely giving up the majority of medicine so you have to be okay with that. There’s a lot more to ophthalmology than you might think so there’s a lot to learn and not too much worrying about the nuances of COPD or heart failure anymore.
- The first year is variable. You might be doing 9 months of wards in IM and 3 months of ophthalmology as a worst case scenario but you also might have effectively a built in transition year.
Day in the life
PGY-1 Intern year – It’s extremely variable and you will definitely do some time on the internal medicine wards (they do this because might never think about most of this again). It could be like any other prelim year or it could be like a transition year (some ER, some outpatient, some electives).
PGY-2-4: Highly variable based on program. Your first year will probably be comprehensive, some specialty exposure (e.g. plastics and retina), a lot of injections, and you might either be not even starting the steps of cataract surgery or be doing cataracts start to finish in January. Really pay attention to how the curriculum is constructed. Call usually gets better as you progress through residency with only backup call the last year.
Call
Call varies wildly between programs. It’s usually every “however big your residency class is” days. That comes out to about once a week day and one weekend a month. Some programs have dedicated night float. In bigger cities call can be pretty busy. In more rural programs call can be lighter. It’s also typically home call so you won’t be stuck in the hospital for days on end.
Fellowships
There’s plenty to do after residency but again, it’s not always necessary. There is a lot of room for sub-specialty though.
Occuloplastics: This is the only “ACGME recognized” fellowship and is also really competitive. You have to apply a year earlier than the rest. Your scope will be surgeries around the eye. Your bread and butter will be fixing droopy eyelids (ptosis), excess eyelid skin (dermatochalasis), and doing botox injections. Your scope will also include more complicated procedures and different things like tarsorrhaphy and debulking for orbital tumors or cellulitis. You’re probably giving up cataracts with this fellowship.
Retina and Vitreous: This is serious business but other ophthalmologists may call you a “taxidermist.” A lot of times you’re the last line of defense for vision. Your bread and butter will be the Pars Plana Vitrectomy (PPV) or the scleral buckle for retinal tears/detachments. You’ll also do a LOT of injections for diabetic retinopathy and you also may handle the really complex cataract surgeries that risk the posterior chamber. You’ll do a lot of pan retinal lasering for diabetes in clinic and even freezing the retina to weld it down until you can do surgery. You’ll be saving some very sick eyes.
Glaucoma: Glaucoma is changing. The big surgeries are trabs and tubes. Now there’s a plethora of MIGS procedures (micro invasive glaucoma surgeries) to buy time before patients need a conventional glaucoma surgery (that have complication rates approaching 50% in some studies). This is a rapidly changing specialty and very exciting that we can now intervene earlier in the disease to prevent further vision loss or at the very least buy time before the bigger surgeries.
Cornea and Refractive/Anterior Segment: Retina may call you “window washers” but if the cornea becomes scarred or opaque, just give them a new one with a corneal transplant. Times are changing in the cornea world also and you don’t always need to do that now. There’s less invasive options like DMEK and DSAEK. Patients will really love you because clearing the “window” of the eye can drastically improve vision. You’ll also manage things in clinic like dry eye, keratoconus, and Fuch’s. Refractive surgeons live to optimize vision. There are many refractive surgeries like LASIK, LASEK, PRK, and the new SMILE.
Pediatric Ophthalmology: Exactly what it sounds like. You’ll have to implement really creative ways of examining kids’ eyes like streak retinoscopy. Your bread and butter will be strabismus surgery and aligning their eyes to prevent vision loss. You’ll also handle juvenile cataracts and the dreaded ROP.
Neuroophthalmology: This is the last “major” fellowship. The weirder things like ischemic optic neuropathy, idiopathic intracranial hypertension, myasthenia gravis, and adult strabismus will be your responsibility if you choose surgical neuroophthalmology. This is one of the less procedural specialties.
Others: There’s other eye specialties like medical retina, cataract, uveitis, and pathology that are about what they sound like. You’d really need to want to practice in a large academic center to get the volume to see some pretty rare ocular diseases.
Early Considerations
Step 1/2
The median Step 1 score for matched applicants is traditionally in the mid 240s (see the 2022 report here) and creeps up every year most recently to 247. Now Step 1 is pass/fail for scores reported after January 26, 2022 (more info here). Without this “great equalizer” programs are almost certainly going to focus on Step 2 as a quick screening tool. For those who will be affected by this (roughly those applying in 2024, the classes will no doubt overlap at first) our personal opinion is to aim for an early Step 2 score of >250. What is the basis of that opinion? >50% of Ophthalmology First Year residents tend to have a Step 2 score of 250 or greater (more info here). SF match appears to already have switched to a “Pass/Fail” entry for Step 1.
Letters of Recommendation (LORs)
Ophthalmology is a small community and programs value the opinion of their colleagues. Leaving a good impression on everyone you work with is important. Good ways to build rapport with faculty who can write letters is proactive and helpful shadowing, research, and involvement with the interest group.
Research
This is more of a “check the box” component but can do a lot for you in other ways. Demonstrating interest in the field through research is important and it is possibly the best way to learn about ophthalmology. Most admission committees are looking for you to have done some Ophthalmology research. Some programs do use amount and quality of research as a metric when making decisions so as always, more tends to be better but make sure you have some. Independent original research is always more highly regarded than case reports. This is also a great way to build relationships with faculty and getting your name out there at meetings can also go a long way. For more help with research, see the Research Info page.
Grades
AOA is strongly associated with matching. Outside of AOA, grades don’t appear to be a big factor because it’s so subjective among medical schools. Avoid failing and other red flags (e.g. in faculty feedback). A couple of honors will definitely help if your school uses that grading system but this appears to be among the least weighted factors. Again, things are changing with pass/fail Step 1 so we’ll see.
Through the Years
M1
Focus on doing well and getting adjusted to medical school. The earliest it’s reasonable to be proactive about ophthalmology is probably the Spring of M1. Many schools have a summer research program and this is the perfect time to get your foot in the door. It would be helpful to start an ophthalmology research project that summer to both learn more about the specialty and start building relationships.
M2
Again, focus on doing well. Honor things if your grading system allows it. You can continue some light research through this time. If your Step 1 is scored focus on that during the spring. Try to get a poster presentation or even publication out of the research you did the summer after M1 year. Every little thing counts.
M3
It won’t hurt to continue research but this is also a time to be trying to honor rotations, especially the surgical clerkships. Consider non-ophthalmology surgeons for one of your letters of recommendation (LORs). This is also the first time you’ll formally rotate through the ophthalmology department. Make a good impression. For more information on basic ophthalmology knowledge and succeeding in clinic as a student visit the Educational Resources page.
M4
Now it’s time to apply. The future of away rotations is uncertain but you should at least do one at a program you’re genuinely interested in or at the major institutions (Duke, Iowa, Bascom) while they’re allowed. It would be great to get a LOR from your away but it’s not necessary. Ophthalmology applications are generally due around early September so consider this for planning. Plan a light schedule for the Fall of M4 to make room for interviews. Ophthalmology interviews will be virtual for the foreseeable future.
Away Rotations
VSAS
VSAS is frustrating and you can’t usually start the process until January of M3. Look up the program requirements and fill out the AAMCAS vaccination record so everything is ready to submit as soon as programs open. Avoid applying to many programs, declining aways can be bad. Away rotations are not competitive so pick programs you’re interested in or want LORs from. I have personally heard stories of programs not extending interviews due to applicants declining aways. Be careful.
Logistics
Schedule the rotations you want a LOR from in July. Away rotations are very expensive because you’ll need a place to stay and a car. The website rotatingroom.com can be used to find someone to stay with for a month. It’s hit or miss but worth looking into early. Facebook and Reddit are sometimes good resources for this but knowing someone in the city will help a lot.
You might not hear from the program about where to meet on the first day and such until a couple weeks before you start so don’t be alarmed. If you want a LOR, make that intention known early so they can anticipate writing it (theirs really needs to be in by the first week of August). You don’t want to be panicking at the last minute and stressing about if you’re letters are all submitted and ready.
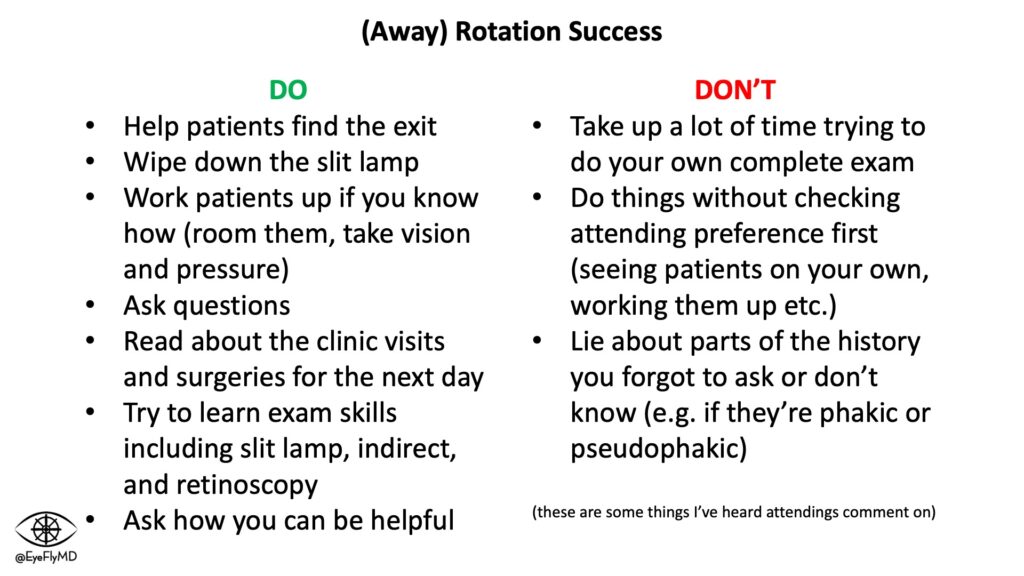
The Rotation
Do your best and read the resources suggested on Educational Resources page if possible and follow our recommended ways to be helpful in clinic. Be helpful and work hard. Keep in mind that doing an elective is a double-edged sword. A program may not rank you (even after a “courtesy interview”) if any red flags were detected during the rotation. Be sure to be the best version of yourself and approach every day of your rotation as a daily interview with anyone you interact with in the clinic and OR. Don’t’ let your guard down.
How to Succeed as a Student
As someone who was there I know it’s difficult to help in the eye clinic sometimes because ophthalmology requires a unique skill set to complete an exam. You can appreciate coarse lung sounds on IM wards but you probably won’t even have the tools to appreciate lattice degeneration on an exam.
Unfortunately medical school is still a game that needs to be played. It’s played most successfully by being perceived as helpful and making the lives of the attendings easier and not introducing any additional stress or problems.
Here are some ways students can be helpful:
- You can show patients the way out of the clinic
- You can clean the portions of the slit lamp that contact the patient (chin rest, forehead rest, applanator, etc.)
- If you know how to take vision and (tonometer) pressure you can help room patients if the clinic gets busy
- Help with odd jobs: walking patients to the ER, walking samples to the lab, looking for ways to generally be helpful, etc.
If you scrub into surgery, your job will most likely be to keep the cornea hydrated with BSS (balanced saline solution). This allows a good view for the surgeon and protects the surface. It seems minor, but here are way to succeed in BSS duties:
- Look for the 3 light reflexes from the operating microscope on the cornea, this will be your best indicator of the ocular surface status. Once these become blurry or distorted the view inside the eye is probably becoming blurry or distorted as well. This will tell you when to squirt.
- Don’t be aggressive, some patients have a sensitive Bell’s reflex and every time you squirt the patient’s eye could roll back. Be aware of this for sensitive portions of surgery (e.g., the rhexis).
- Don’t be so overzealous it actually interferes with the surgeon’s view. Constantly wetting the cornea can be distracting.
You want to very much avoid things that could slow down clinic like doing your own very thorough exam. You can always ask attending preference or ask residents what the attending likes.
Preparing the Application
The 2022 cycle timetable from the SFMatch website is below:
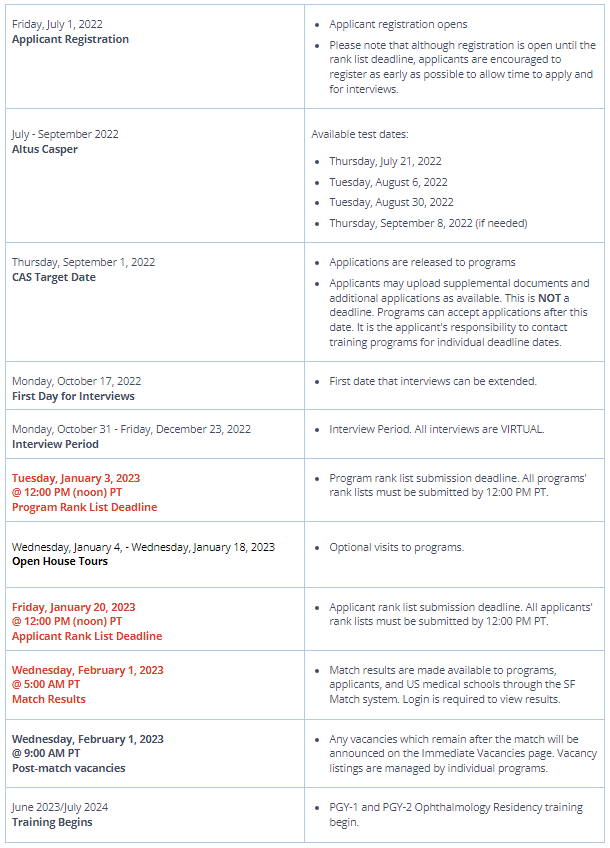
Or, a prettier version from AUPO:

Think about the application early. Have your CV ready early and tell your home letter writers to have the letters finished early (tell them “by June 1st”). The application process happens fast so anticipating is important and being able to just copy and paste things over will help especially if you’re in the middle of away rotations or studying for Step 2.
Altus Suite
During the 2022-23 match cycle the AUPO has introduced another aspect for the ophthalmology match: The Altus Suite. The Altus Suite is the examination service that administers the Casper test, Snapshot, and Duet Assessment. The primary reason behind introducing these tests is to gain insight into an applicant’s values and ethical problem solving without rehearsal or revision. With the rise in number of applicants and loss of Step 1 as a “universal metric”, this is meant to serve as a way to identify individuals who best align with their program’s mission and core characteristics.
It is uncertain how much weight is being placed on these assessments or how they are being used to select applicants for interviews. Nonetheless, applicants should be prepared to reflect on their experiences and qualities they deem important to the foundation of their character.
Having applied to medical schools relatively recently, most applicants may be familiar with the Casper test and the nature of the questions and the test taking process.
The Casper Test is a 2-hour long examination wherein the examinee is faced with a variety of ethical dilemmas some being medically oriented. The applicant has 5 minutes to answer three open ended questions that will be assessing for these qualities:
- Collaboration
- Equity
- Communication
- Empathy
- Ethics
- Motivation
- Problem solving
- Professionalism
- Self awareness
- Resilience
The challenge with this assessment is to concisely respond to these prompts while incorporating these listed qualities. Luckily, the Altus suite provides a practice test. After the exam is completed, it is sent off and scored where applicants will be placed into a quartile based upon evaluation of each of the stated characteristics.
The Snapshot is a short one-way interview that asks general interview questions which allows a minute for a video response to a scenario. Be prepared to answer questions about personal qualities or how you would respond in a professional scenario. It is very important that you dress professionally and look presentable just as in any interview as programs have access to this.
The Duet Assessment is where an applicant has a chance to voice their opinions about what qualities they value in a residency program. The qualities vary from resident wellness initiatives to research and publication opportunities. Programs will also complete this assessment and can help pair students whose values align most closely with that of the program.
Each component of these set of assessments is designed to help interview committees better understand the applicant as a person prior to offering an interview. It appears that programs are evaluating applicants on how they would fit into the culture of the program to help focus their interview process.
Curriculum Vitae
Keep this updated throughout medical school so it’s ready to go. You will also be pasting portions of this into the application portal.
Here is a CV template I’ve been complimented on for its cleanliness.
Personal Statement
The personal statement now consists of a short “autobiographical sketch” and answering 2/4 essay questions. The instructions from SF match are below:
“Write an autobiographical sketch (summary of your life, who you are and your aspirations) not to exceed 500 words and answer 2 of 4 of the essay questions below (essay questions not to exceed 250 words each). Select 2 questions from the list below. Copy the 2 questions and limit each answer to 250 words.
1) What does resilience mean to you? Describe a situation in your personal or professional life where you have demonstrated resilience.
2) Describe an important mentor and relate how that person has been helpful to you.
3) Describe a way in which you will add diversity to your residency class. This may relate to your background, upbringing, life experiences, professional/personal interest, or educational path.
4) If you were to start an ophthalmology residency program, what would be the three core values you would base it on?”
I included my personal statement because I received good feedback on it. Just remember the instructions have changed since I applied and plan to answer this portion as above.
Outside Interests and Hobbies
THIS IS POSSIBLY ONE OF THE MOST IMPORTANT PARTS OF YOUR APPLICATION. The majority of things you will discuss during interviews will come from here. Include a lot of things but make sure you are familiar with them. Definitely list playing guitar if that’s true but don’t be surprised if you’re asked to play something during interviews.
Education/Publications/Poster Presentations
These are self-explanatory sections
Career Objectives
This is a small section that requires some generic entry. I’m not sure if programs really even read this. Mine was:
“I aspire to practice as a patient-centered, compassionate, innovative, and technically proficient ophthalmologist. I will remain open-minded with regard to the details of my career but plan to continue my passion for research and the most up to date evidence-based approaches to ocular surgery.”
Specialty electives and related activities
There will be a section where you’ll need to describe the ophthalmology electives you’ve taken and your experience in them. Says something like “In this 4-week rotation I spent time with X and did Y and Z…”.
Public service and activities
Copy this from your CV.
Letters of Recommendation
Tell your letter writers (generally recommended to be 2 ophthalmologists and 1 IM/General Surgery) to have the letter ready by June 1st. You’ll put their info into SF match and it will send them a link to upload it. If you’re anticipating one from an away make sure they know early so it can be uploaded by the first week of August. Being well ahead of this will save you a lot of anxiety later.
Ophthalmology is a small field and letters carry a lot of weight.
Interviews and Interview Season
I highly encourage all applicants to participate in mock interviews. This also gives you a chance to practice answering the common questions you know you’ll be asked. Make sure they never sound rehearsed. To avoid answers from sounding too “canned” it’s helpful to memorize an outline of how you’ll answer the questions.
Also, read about the program and city so when they ask about why you chose to apply there you have some things to talk about and you can demonstrate genuine interest.
Lastly, review your own CV and application before the interview so if you’re asked about a research project it doesn’t catch you by surprise that you were even involved. Make sure you’re able to give a quick summary of your role and the results of any research you list. Some interviewers really lean into this.
Keep Track of Things on Interviews
I would suggest making a list of things that are important to you (e.g. location, surgical numbers, call, etc.) and keep track of these particular items during interviews. It will help you keep things straight when you make your rank list later.
What to look for in a program
- Early cataract surgery exposure and good surgical volume. This is the bread and butter procedure of ophthalmology and it helps to be exposed to it early. Residents are required to do 86 cataract surgeries but I’ve often heard 200 is about where you feel comfortable on your own (obviously this varies from individual to individual). This means 200 would be a good target number for programs. I mention this again later, but don’t ask about this directly. It’s considered impolite.
- Fellowships are well represented. Most programs will have a Retina, Glaucoma, and Cornea service. Not a lot of places have ocular pathology for example and you can learn a lot of from them. At least make sure someone is on faculty for the major specialties (including oculoplastics and neuroophthalmology).
- Call and curriculum. Some programs have a lot of one-on-one time with the attendings and some programs are more sink or swim program and some programs are both. Some places do blocks and some places just have you spend a day of the week on this service then that service for example. Try to imagine about what would fit your learning style best. As always, think about how important lifestyle is to you.
- Class size. There’s a sweet spot between 4-6 residents. 2 is probably not enough because that means frequent call even if the program is less busy. 10 might mean less frequent call but should tell you something about how busy the program is and the 10 might be divided over multiple sites. The division of call is important to ask about.
- The intern year. Know what you’re getting into the first year. This can greatly impact lifestyle if that’s important to you.
Number of Interviews
The number of interviews you should attend is extremely subjective. Essentially, go to every program you are actually interested in. There are a lot of figures floating around about how many programs you need to rank to match but it varies and depends largely on the person. A candidate can interview at 3 places and really click with a program and match. Another candidate can interview at 19 places and leave a bad impression every time and not match. Don’t get too hung up on those figures. Because you’re wondering, the “magic number” is generally regarded as around 9. Ranking about 9 programs confers a high probability of matching based on historical data. Attending 10-12 interviews is reasonable and is usually the aim based on the AAO. Only go to that many if you’re interested in all of them. 15 is getting to the upper limit of reasonable where scheduling and money (in the time of physical interviews) become difficult. Always keep in mind the individual is much more important than historical statistics and these statistics don’t necessarily apply to the individual.
Virtual interviews have a cap. Currently, applicants can accept 15 interviews. This was reduced from 20 the first year of virtual interviews and 18 the second year. The “safe number” may change but we don’t have enough data in the virtual landscape yet.
Virtual Interviews
As mentioned earlier, interviews will be virtual for the foreseeable future. As ridiculous as it may sound at first, a ring light is a worthwhile investment. It allows soft lighting and a more professional look. A nice webcam wouldn’t be a bad idea either. Also, pick a spot that has a nice clean, plain background. Use whatever you can to your advantage in these virtual interviews. Programs are more likely to remember the applicant with a well lit and professional appearing presentation compared to an applicant appearing on a small, grainy screen in the dark.
Having something relevant to your interests nearby/on the wall behind you can help you stand out. An example is having paintings you’ve done or photographs you’ve taken hanging behind you. Plants have been popular and also look pleasant.
Socials
With virtual interviews, social events were not as common. Many are the night before, but other were scheduled randomly before or after the interview date. If multiple dates are offered, try scheduling it before your interview. These events can help you learn a lot about a program and may provide some additional questions to ask faculty during your interview. Don’t be afraid to reach out to current residents for more information before the interview just be tasteful with how you do it.
Interviews/Interview Questions
These are examples of common questions I remember as well as questions I had for the faculty and residents. You will likely be asked “What questions do you have?” with remarkable frequency. It’s helpful to have some things ready to ask to minimize the inevitable awkward silence over virtual interviews.
I cannot emphasize enough the importance of having simple and positive questions ready to go for when you’re inevitably asked this by everyone throughout your interview experience. Examples of these fast, positive, and benign questions are: “What’s your favorite part of the program/city?” “How frequently do the residents work with medical students?” “What upcoming changes are you excited for?”
A big question pro-tip is it’s better to stand out and be memorable especially in this zoom situation. Ask questions in the lobby, appear engaged, and show that you know something about the program (e.g. the you read the website) and are eager to learn more. Avoid going through any Zoom lobbies without acting engaged if possible. Zoom is impersonal/awkward and you have 3-4 hours to make a good impression on programs.
| Be Prepared to Answer | Questions for Faculty | Questions for Residents |
|---|---|---|
| Tell me about yourself. | What are you looking for in a candidate? | What does a day in clinic look like? |
| Why did you choose ophthalmology? | What is the breakdown of your preliminary/intern year? | What is the call schedule like? |
| Tell me about <some aspect of your application, CV, etc.>. | Where do most residents go after residency? Private practice or fellowship? | How many cases are you paged on per night? |
| What do you do for fun? | Are there many opportunities for research? What kind of research can I expect in this program? | Which areas of the city do most residents live? What is the average rent? |
| Why are you interested in our program? | How many hospitals participate in this residency program? | What are your favorite and least favorite things about the program? |
| Where do you see yourself in 5/10 years? | Are there opportunities to teach medical students? | Do residents socialize and get together often? |
| Are you interested in pursuing a fellowship? | Where do you see the program in 5/10 years? | Does the program cover lenses, books, and the question bank? |
| If I asked your friends to describe you, what would they say? | What upcoming things are you excited about for this program? What changes have been made recently? | Does the program cover conference travel? |
| If you were to describe yourself in 3 words, what would they be? | What is your favorite part about this program? | What is the didactic schedule like? |
| Tell us about an interesting case you have seen and how it influenced you. | What are your favorite parts of the city? | How many call sites do residents cover? |
| What are your biggest strengths and weaknesses? | Are there formal mentorships with faculty? | What is something unexpected about the program? |
| Why would a Midwest/Coastal person like you move to the Coast/Midwest? | Which department do you think is the strongest? | Do you feel comfortable asking for help during call? |
| What are you looking for in a residency program? | How is grand rounds structured? | What role do fellows play in your education? |
| What sets you apart from other candidates? | ||
| What is your biggest failure and how did you handle it? | ||
| What are you most proud of? (inside and outside medicine) | ||
| What did you find interesting in medical school other than ophthalmology? | ||
| What leadership positions have you had? | ||
| How do you deal with stress? | ||
| Who is the person you most admire? What 3 people living or dead would you want to have dinner with? | ||
| Tell me a joke. Teach me someting. | ||
| What is your plan if you don’t match? | ||
| If you couldn’t go into medicine, what would you do? | ||
| If there is one thing you could change in your past, what would it be? | ||
| How would your spouse feel about moving to this city? | ||
| Explain <poor grade or Step score in your application>, | ||
| What was your favorite (or least favorite) job and why? |
Special Note on Courtesy with Questions
Avoid directly asking about surgical numbers. This is one of the games you have to play. Find out some other way. Asking about case numbers directly is considered tacky for some reason. Programs with good numbers will publish them or make it part of their presentation. If numbers are not included in any of the program’s information then…
Thank You Notes
After the interview it is courteous but not expected to send a thank you note in some form. An email sent to everyone who interviewed you (don’t forget to thank the program coordinator for their organizational effort) is more than enough. I would suggest making them personalized in some capacity and writing something about something you enjoyed about the program or the city. A copy and paste job might not be the best look. Again, these aren’t expected and won’t influence everything but it’s a nice thing to do. In the impersonal Zoom world I would personally do everything in your power to stand out and make an impression.
Open House
A new feature of virtual interviews is the opportunity for applicants to visit programs after programs submit their rank list and before applicants submit their rank lists. This means programs cannot be swayed by which applicants choose to visit them and applicants can collect any additional data they need before submitting their rank list. These visits are optional and vary greatly depending on program.
Spreadsheet/Discord
There is an infamous google spreadsheet or Discord Chat every year where applicants can talk to each other and post impressions of programs as well as their stats as interview season progresses. It also lists the impressions of programs based on last year’s interviews and this can be a good way to know what to expect. Try to avoid getting tied to this though as the applicant numbers are very skewed and it paints an unrealistic picture most of the time. You can find it by googling “Ophthalmology Spreadsheet [MATCH YEAR]”.
Doximity Rankings
Be careful putting too much weight in these as there is some politics involved. An AAO article brought up these points about program ranking:
- “By engaging in every aspect of the process from soliciting nominations to marketing results, we provide a tacit endorsement of the ranking results that undermines the credibility of our profession”
- “there is no consensus on which outcomes measures should be used to assess performance in ophthalmology.”
- “There is no valid way to rank ophthalmology residency programs, and academic departments should refuse to participate in any process that attempts to do so.”
Basically, don’t get too hung up on this. There are some obviously research-heavy and traditionally prestigious programs with “famous” faculty like Bascom Palmer, Wills, Wilmer, Duke, Iowa etc. and there’s also some programs with qualities that could give you a sub-optimal training experience (e.g. no VA, minimal faculty) and these are not always reflected in the rankings. It’s really important to think about your personal career goals and what you are looking for in a program. Factor in location, family, fit, culture, and what the program has to offer more than prestige.
Ranking and Matching
General Advice
Try not to think about the flawed ranking system when making your list. Go with your gut and consider the things that were important to you. Keep track while interviewing of pros and cons about each program. They’ll all blend together so it’s important to take notes in real time. Some things that are generally beneficial in a program include high primary cataract volume, a VA, and good fellowship matching history.
Ranking
Keep track of what you liked and didn’t like about programs as you interview. Pick a couple things (e.g. surgical volume, location, faculty etc.) that matter a lot to you because that may be a good jumping off point for your final list. In the end, nothing beats gut feeling when it comes to making the list. Think about the experience you would have at each place and how it matches with the experience you’re looking for.
There is no way to “game” the system so rank in order of your true preference. Don’t try to throw in a few “safe” programs toward the top just in case. Truly rank in order of your genuine preference. This video explains the ranking algorithm.
As you probably know, ophthalmology matches much earlier than the other specialties. This has been delayed in recent years but early February is when you can expect the match email at 7 or 8 AM on a Monday morning.
Re-Applying
Introduction
In the TV Series Star Trek: The Next Generation, Captain Jean-Luc Picard said, “It is possible to commit no mistakes and still lose. That is not a weakness. That is life.” Sometimes things don’t work out like we hope for but it doesn’t mean it’s over and we should give up. One of our contributors, Mia Koci, didn’t match her first cycle but then successfully matched the following year. This section consists of her advice in her own words if you find yourself in a similar situation. Hopefully her success is comforting.
I’ll turn it over to Mia:
The match rate for ophthalmology was ~80% for US Allopathic seniors in 2021, and that percentage decreases to 74% if you include graduates, IMGs and US Osteopathic seniors. In 2020 I was one of those ~20% who didn’t match, and navigating that process was overwhelming, confusing, and there were no good resources. I felt like I was on my own. Hopefully this overview can give some peace of mind, comfort, and hope if you have found yourself in the same situation. That being said, this guide is based on my personal experiences, opinions, and research and is by no means all encompassing.
Firstly, I want to emphasize that this result does not speak to who you are as a person, applicant, your work ethic, or likability. Take time to be angry, frustrated, and sad. Lean on your support system, family, and friends. No one will really understand what is like but know that there are people that care about you and are rooting for you.
First Steps:
- Set up appointments with your home program and school deans
- Email PDs and coordinators at places you interviewed and ask for feedback
- Weigh your options which include reapplying ophtho, submitting a rank list for a specialty you may have dual applied into, SOAP into alternative specialty or prelim year
Important Questions When Considering Reapplying:
- How many interviews did you receive this year?
- What were the weaknesses on your application? Would an extra year of research, experience, or developing connections help overcome those weaknesses?
- Do you have the financial means to delay residency?
- Did you dual apply? Would you be happy and fulfilled pursuing another specialty?
Ophthalmology Related “Extra Year”
If you decide to pursue a research year or pre-residency fellowship related to ophthalmology with the goal of reapplying, here are some tips based on experience. First, update your CV as soon as possible and contact your letter writers. Many of the program applications required a program specific personal statement/cover letter, updated CV, and letters of recommendation, while others simply asked for a copy of your completed SF Match application. Apply to as many programs as possible, especially given the competitive nature of the high-quality, reputable pre-residency programs that others in the same position will be applying for.
Finding these programs can be difficult, and a good resource is listed below. Reddit, SDN and the Ophthalmology Match Google Spreadsheet are additional resources where similar positions are posted yearly, usually by the students who have completed them and are looking for their successors. While not all programs are created equal, a very beneficial thing to emphasize when interviewing the second time is dedication, commitment, and skills that the research year provide that would be applicable to residency (effective patient communication, teamwork, problem solving, and applying evidence-based medicine). There is an aspect of gaining mentorship and making connections that could increase your interviews and chance of matching at a program as well, so something to take into account.
Things to Look For in a Program/Research Year:
- Is the program associated with a residency?
- Does the program have a strong track record for matching re-applicants?
- What would mentorship look like throughout the year?
- Is there the possibility of a strong letter of recommendation?
- What is the start date and end date?
- Is there potential to complete a project/paper prior to the application due date or start of interview season?
Prelim or Transitional Year Internship
Starting intern year by matching into a medical or surgical prelim year or transitional year with the goal of reapplying has worked for others in the past as well. This has become more complicated with almost all ophthalmology programs becoming joint or integrated and there is a high likelihood you will be required to repeat intern year. There is less flexibility with time off for application preparation and scheduling interviews. However, this may be a good choice if you are unable to secure a paid research or pre-residency fellowship position. There is something to be said for someone who is able to manage the workload of intern year while still able to commit to the entire reapplication process as well.
Graduation
Mia was able to delay her medical school graduation and was granted a “leave of absence” to pursue the research year, which was helpful in several ways. Her school administration readily worked with her, she didn’t have to pay tuition, and she was still able to get health insurance through the school. Additionally, since she was still considered a USMD senior, she got far less interrogation during interviews to her backup specialty. Some colleagues in similar situations had graduated and because of their MD status, questions about “what happened last year?” would come up often. This isn’t an issue if you have a well-developed explanation for “well why X specialty now?” Never be dishonest about dual applying but it is a more difficult situation to navigate as no specialty wants to feel like they’re a “second choice.” Lastly, if you aren’t planning on SOAP or matching into a prelim year this year, you need to withdraw completely from ERAS and NRMP. That way next year, there will be no record of your application as far as programs can tell and it will look like your first time applying which is helpful.
Unfortunately, there’s no perfect formula or guarantee when it comes to reapplying. The match is also unpredictable and people with very few interviews match and people with the “ideal” number of interviews don’t match. Take some comfort in knowing it only takes one program to match. If being an ophthalmologist is your passion, what’s one more year in the grand scheme of your career? If you are able to approach the year with strategy, a solid backup plan, and openness about your growth and progress from the experience, I think it’s worth going through the match again. That being said, everyone’s situation is unique and discussion with your administration, friends and family should help guide what is the best next step for you. This is an unpleasant part that nobody likes to think about but hopefully this has been helpful, and if you have your own questions, comments, experiences, or resources we would love to hear from you.
List of Pre-Residency Fellowships
Other Matching Resources
These are many other good resources you can use so don’t take our word for it. It’s also important to find a mentor and advisor early so you can always have different perspectives from an actual ophthalmologist on this process. If anyone needs advice, just reach out to me and I’m happy to help however I can. I think a special strength of this Matching Guide is we are not speaking on behalf of any official authority so we have spoken freely and reflected our feelings and experience without any reservation. That being said, here are other resources from official organizations: